
Patient Reported Outcome Measures (PROMs)
We measure and analyze the subjective perception of treatment success. This allows us to constantly optimize the quality of our treatment.
Patient Reported Outcome Measures (PROMs) aim to increase the quality of treatment as perceived by our patients and thus place them at the center of our efforts.
PROMs are sets of questionnaires that focus on the general state of health but also specifically on the respective illness and the consequences of its treatment. This makes it possible to measure quality of life and health status in a long-term and standardized manner.
The survey is completely digitalized. This means that the individual details and the resulting findings are available to medical staff in real time. This allows them to react promptly to changes in the patient's state of health and quality of life. The data can also be analyzed for patient groups - for example, to compare different treatment methods. The aim is to generate added value for our patients in line with the USB "Value Based Healthcare" strategy.
In 2023, the USB made significant progress towards value-based healthcare in two innovative collaborations with health insurers and partner hospitals.
The current remuneration system based on flat rates per case offers false incentives. This means that service providers earn more the more cases they treat. However, the quality of treatment is not yet reflected in the so-called flat rates per case.
The inclusion of quality indicators and PROMs is intended to counteract this. The primary aim is to remunerate the quality provided and not just the quantity. The aim is to prevent unnecessary interventions and achieve the best possible treatment outcome. PROMs are a central component of this, as they enable long-term measurement of the success of treatment from the patient's central perspective and therefore allow a statement to be made about the individual necessity of the intervention. They also allow early detection of any deterioration in the subjectively perceived state of health.
Innovative Vergütungsmodelle durch Nutzung von PROMs
The survey is completely digitalized. This means that the individual details and the resulting findings are available to medical staff in real time. This allows them to react promptly to changes in the patient's state of health and quality of life. The data can also be analyzed for patient groups - for example, to compare different treatment methods. The aim is to generate added value for our patients in line with the USB "Value Based Healthcare" strategy.
In 2023, the USB made significant progress towards value-based healthcare in two innovative collaborations with health insurers and partner hospitals.
The current remuneration system based on flat rates per case offers false incentives. This means that service providers earn more the more cases they treat. However, the quality of treatment is not yet reflected in the so-called flat rates per case.
The inclusion of quality indicators and PROMs is intended to counteract this. The primary aim is to remunerate the quality provided and not just the quantity. The aim is to prevent unnecessary interventions and achieve the best possible treatment outcome. PROMs are a central component of this, as they enable long-term measurement of the success of treatment from the patient's central perspective and therefore allow a statement to be made about the individual necessity of the intervention. They also allow early detection of any deterioration in the subjectively perceived state of health.
Further information on the projects with regard to remuneration models can be found here:
Further information on the implementation and use of PROMs can be found here:
Use and benefits of PROMs
- at an individual level in patient contact
- at a collective level as a quality indicator
- as a building block in the development of quality-based remuneration models
PROMs: A patient's experience
What are patients' experiences with Patient Reported Outcome Measures (PROMs)? How is the survey perceived? A breast surgery patient who was treated for breast cancer at the USB gives us an insight.
"When I filled out the questionnaire for the first time, I was amazed at the sometimes intimate questions that were asked. (...) But after the second or third time, you get used to it. It can perhaps happen that patients find it too intimate. But I think you (...) don't have to be ashamed. The interviews can help (...). (...) at first you're shocked anyway that you're ill and how ill. And then comes the interview and you've never been confronted with such an intimate interview before. And over time you understand why the questions are being asked. Because after a while you understand exactly what they mean, because you can understand it. (...) When you're in the middle of it, you just work. (...) It's only with time that the questions take on depth, i.e. meaning."
"(...) the professionals have a very broad knowledge (....) But nevertheless, the questioning that they do (editor's note: this refers to PROMs) is also a little different. It is more personal. So you can also discuss it. For example, if something doesn't improve, what's the reason and so on."
The Clinic for Orthopaedics and Traumatology records PROMs for:
- Patients with planned orthopaedic surgery on the hip, knee, foot and shoulder
- Traumatology patients who require surgical treatment due to a bone injury ("fracture") of the upper and/or lower extremities.
- upper and/or lower extremities who require surgical treatment.
- Patients with a musculoskeletal infection
The examples (Fig. 1 and 2) show the improvement in the physical functioning of patients who have received a joint replacement by means of a prosthesis due to their hip or knee complaints.
The KOOS-PS (KOOS-PS: Knee injury and Osteoarthritis Outcome Score-Physical Function Short Forms) (for knee patients) and HOOS-PS (HOOS-PS: Hip Disability and Osteoarthritis Outcome Score Physical Function Short Forms) (for hip patients) measure the values ("scores") formed from various questions Bilici, M et al. (2021). Outcome measurement in trauma surgery with a fracture database and clinical and patient-reported outcome measures (PROMs) Bilici, M et al. (2023). A clinical fracture registry for quality assurance Geese, F. (2023). Exploring the Potential of Electronic Patient-Reported Outcome Measures to Inform and Assess Care in Sarcoma Centers: A Longitudinal Multicenter Pilot Study Nüesch, C., Ismailidis, P. et. al. (2021). Assessing Site Specificity of Osteoarthritic Gait Kinematics with Wearable Sensors and Their Association with Patient Reported Outcome Measures (PROMs): Knee versus Hip Osteoarthritis 15 the extent of subjectively perceived difficulties experienced by patients due to their hip or knee pain. The score can have a value between 0 and 100, with a higher value indicating greater difficulties.
In order to measure the success of the treatment, the initial survey is carried out at the USB before the planned hip or knee surgery. This is followed by further postoperative surveys at defined times after the treatment:
- six weeks postoperatively
- three months postoperatively
- six months postoperatively (only for knee patients)
- one year postoperatively
Fig. 2: HOOS-PS score, internal data analysis
Fig. 2: HOOS-PS score, internal data analysis
The gastroenterology department at Clarunis - University Abdominal Center Basel (USB site) - systematically records PROMs for patients receiving infusion therapy for chronic inflammatory bowel disease (IBD).
Patients receive infusion therapy approximately every six to eight weeks and answer the IBD control questionnaire. This records the extent of disease control based on various areas:
- Disease activity
- Change in bowel symptoms
- Symptoms of the disease
- the need to discuss treatment options, symptoms and side effects with the attending physician
The score can have a value between 0 and 16, with a higher value indicating better control of the bowel disease. The aim of treating chronically ill patients is to keep disease activity low and disease control as high and stable as possible.
As the majority of patients had already received infusion therapy when PROMs was introduced for IBD, the first survey does not necessarily reflect the start of therapy. It can be observed that the value remains stable in the patients and increases over time. Patients also have the opportunity to indicate whether they find the current treatment of their disease helpful. If necessary, this information can be used to respond promptly to various aspects of the illness. The graph shows that patients find the current treatment helpful.
Fig. 3: IBD Control 8 score, internal data analysis
At the Sarcoma Center, patients with a sarcoma (rare tumor disease originating from the supporting or connective tissue) are included in the PROMs survey.
The survey dates are:
- baseline
- after completion of neoadjuvant therapy (preparatory drug therapy, e.g.
- chemotherapy before planned surgery, if performed)
- six weeks postoperatively
- three months postoperatively
- six months postoperatively
- one year postoperatively
Various aspects were discussed in the survey, including the physical function of the affected extremity using the TESS questionnaire (Toronto Extremity Salvage Score).
Patients with sarcoma can experience physical impairments as a result of treatment; the TESS measures the severity of the subjectively perceived physical limitation. It has been shown that one year after the start of treatment, patients have regained their original functional capacity or even show slightly improved values.
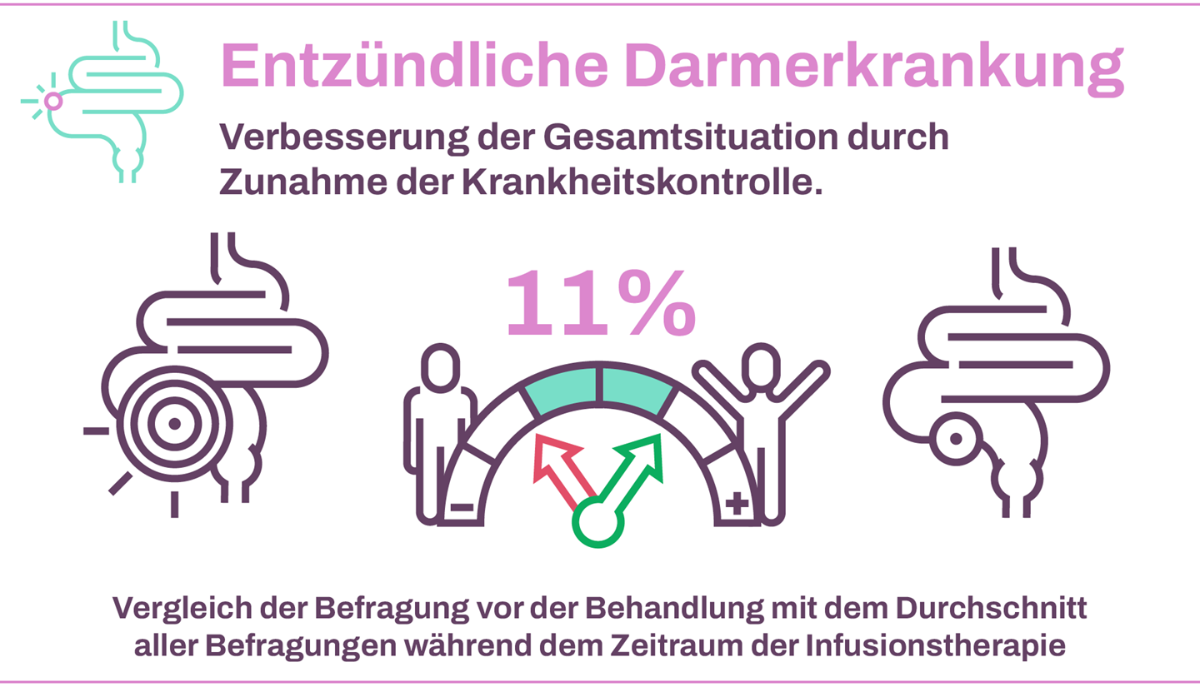
Fig. 5: Toronto Extremity Salvage Score: Physical function, internal data evaluation
Publikationen zum Thema PROMS am USB
