
Hospital-wide indicators
We compare our performance with other hospitals in (inter)national measurement programs. At the same time, we are introducing new key figures within the hospital to make the quality provided in our clinics and departments even more transparent. What is particularly important here is that we record the quality indicators digitally and as automatically as possible and then evaluate them. In this section you will find the results of our hospital-wide quality measurements.
Qualitätskennzahlen sind klar definierte, statistische Messgrössen zur Bewertung der Qualität eines Prozesses oder einer Leistung. Solche Messgrössen sind die Grundlage für eine kontinuierliche Überwachung und Verbesserung der medizinischen Behandlungsqualität eines jeden Spitals. Da Qualität ein komplexes Konstrukt ist, werden stets mehrere solcher Messgrössen oder «Kennzahlen» kombiniert, welche jeweils einen Aspekt der Qualität beleuchten.

Case numbers, complication and mortality rates
The USB is a founding member of the IQM Quality Medicine Initiative. This initiative, which is supported by over 500 hospitals in Germany and Switzerland, has been promoting the quality and transparency of medical treatment for 15 years. Based on routine data, IQM calculates the number of cases, complication rates and mortality rates per hospital for a large number of diagnoses and procedures. The hospitals compare their results with each other and can initiate improvement measures where necessary through targeted exchanges with experts as part of peer reviews.
About the key figures:
You can find our IQM case numbers, complication and mortality rates here.
Infections acquired in hospital
In order to record hospital-acquired infections, the University Hospital Basel has been conducting an annual prevalence survey since 1999. The survey takes place on a specific date on which all patients hospitalized on this date are examined for hospital-acquired infections.
Key figure: rate of hospital-acquired infections (proportion of patients with hospital-acquired infections per 100 patients)
In 2022, the proportion of hospital-acquired infections in the key date survey was 6.0%. This puts the University Hospital Basel in line with the Swiss average (5.9%).

Source: Report Prevalence of nosocomial infections at the University Hospital Basel in June 2022; University Hospital Basel, Clinic for Infectiology & Hospital Hygiene. Coverage of all wards excluding: emergency ward, haematology isolation ward, crisis intervention ward, eye clinic, nuclear medicine; Swissnoso, Point Prevalence Survey 2021 of healthcare associated infections and antimicrobial use in Swiss acute care hospitals; Swissnoso, Second national point prevalence survey of healthcare-associated infections and antimicrobial use in Swiss acute care hospitals (2022)
* No measurement was carried out in 2020 due to the COVID-19 pandemic.
Postoperative wound infections
After surgery, undesirable infections of the surgical site or wounds can occur. Such wound infections can vary in severity, but always represent an undesirable complication that can also lead to a prolonged hospital stay.
In Switzerland, wound infections following surgery are recorded by all hospitals for selected operations as part of a national measurement program (swissnoso).
Key figure: post-operative wound infection rate (proportion of patients with post-operative wound infection per 100 patients)
At the USB, we have been monitoring wound infections after gallbladder, colon and cardiac surgery for several years. The following table shows the wound infection rate for the last three years.
As part of the swissnoso national measurement program, the results are also compared with all other hospitals. You can find the data here.
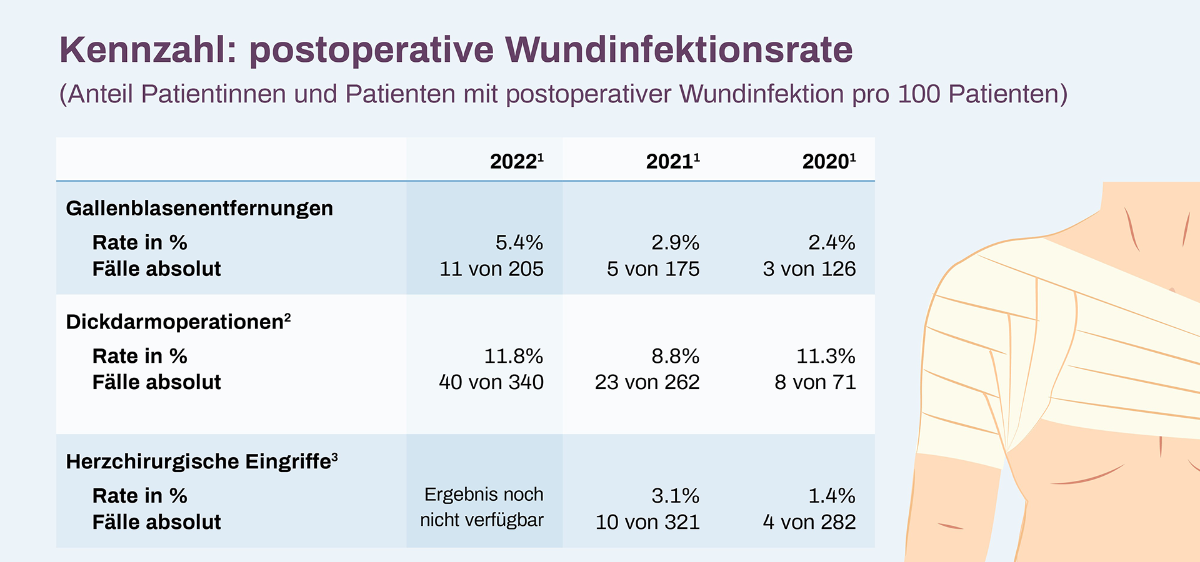
1) The measurement of wound infections was suspended for several months in 2020, 2021 and 2022 due to the COVID-19 pandemic, as a result of which the number of reported procedures is lower in some cases than the actual number of procedures performed.
2) From 2021, the infection rates for colon surgery are reported as a total figure for Clarunis - University Abdominal Center Basel (the St. Claraspital and USB sites)
3) Cardiac surgery procedures up to mid-2021 were tracked for one year, now only for 90 days (change in Swissnoso's national measurement methodology). The results for cardiac surgery procedures in 2022 were not yet available at the time of publication of this quality report, as the follow-up period (90 days) had not yet elapsed for all procedures from 2022.
Decubitus
A pressure ulcer, also known colloquially as a bedsore, is "localized damage to the skin and/or underlying tissue as a result of pressure or pressure in combination with shear forces. A pressure ulcer usually occurs over bony prominences , but can also be associated with medical devices or other objects" (according to EPUAP, 2019). Depending on the severity, pressure ulcers can be divided into four categories, from category 1 (redness that cannot be pushed away) to category 4 (complete tissue loss).
Pressure ulcer rates are internationally recognized as an indicator of the quality of care. Pressure ulcer prevalence measures the frequency of pressure ulcers acquired in hospital and thus provides a basis for quality improvements within prevention.
The USB has a comprehensive pressure ulcer prevention program, which is managed by experts from the nursing/MTT department.
Key figure: Pressure ulcer prevalence rate (proportion of patients with pressure ulcers per 100 patients)
In 2022, 866 out of a total of 30,741 patients developed pressure sores. This corresponds to a pressure ulcer prevalence rate of 2.8%. If pressure ulcers are only considered from category 2 or higher, i.e. cases in which there is actually a partial loss of skin, the pressure ulcer prevalence rate is 1.3%. Pressure ulcer prevalence has been trending downwards since the start of continuous, year-round measurement at the USB.
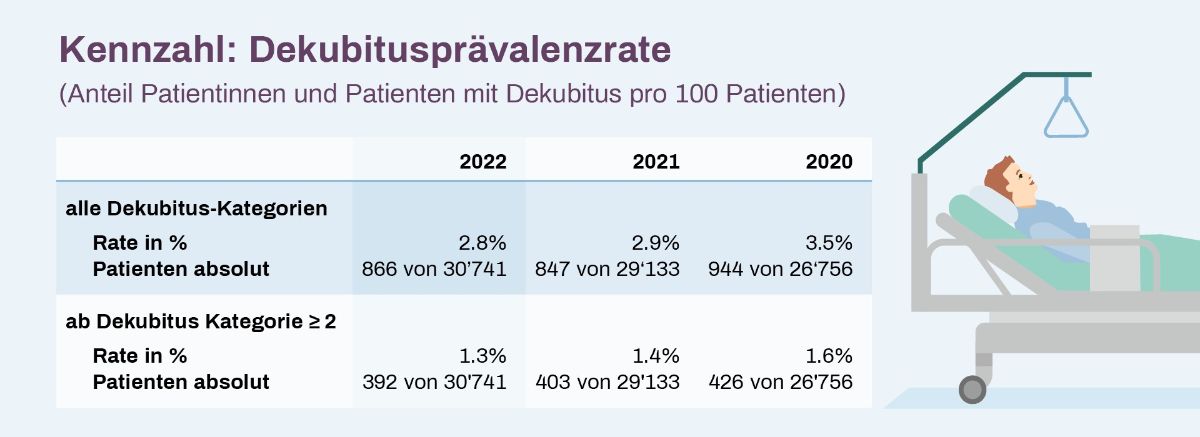
Source: USB, internal evaluations of all wards excluding: day clinics, emergency center, maternity ward, mother-child ward, intensive care unit and IMC (other recording system)
Fall
By definition, a fall is "an event as a result of which a person unintentionally comes to rest on the ground or on a lower level".
We have been automatically determining the prevalence of falls at the USB on an ongoing basis for several years and mapping them in a quality dashboard. Every fall event is documented by the treatment team in a fall log, discussed and evaluated with regard to necessary measures. In addition, the USB has a hospital-wide fall prevention programme that is committed to the continuous optimization of fall prevention measures.
Key figure: fall prevalence rate (proportion of patients with falls per 100 patients)
In 2022, 2.4% of patients fell during their hospital stay.

Source: USB, internal evaluations of all wards excluding: day clinics, emergency center, maternity ward, mother-child ward, intensive care unit and IMC (other recording system)
Use of bladder catheters
Various medical reasons may require the use of a urinary catheter. However, in order to avoid undesirable side effects (e.g. urinary tract infections or injuries) as far as possible, it is important to use bladder catheters as little and as briefly as possible.
One indicator used to monitor the use of urinary catheters is the so-called urinary catheter utilization rate. The lower this rate is, the lower the use of urinary catheters (less frequent and/or shorter).
At the USB, the bladder catheter utilization rate is calculated and mapped automatically based on the nursing documentation. However, it should be noted that the use of urinary catheters cannot always be prevented and that there are areas in which urinary catheter use rates are necessarily high for medical reasons (e.g. in intensive care units or for urological diseases). The comparison of bladder catheter usage rates between hospitals is therefore only possible to a limited extent and is always intended for comparable specialties.
Key figure: Bladder catheter utilization rate (proportion of catheter days per 100 patient days)
In 2022, the average bladder catheter usage rate for all departments was 14.0%. In other words, a patient who is hospitalized for ten days wears a urinary catheter for an average of 1.4 days.
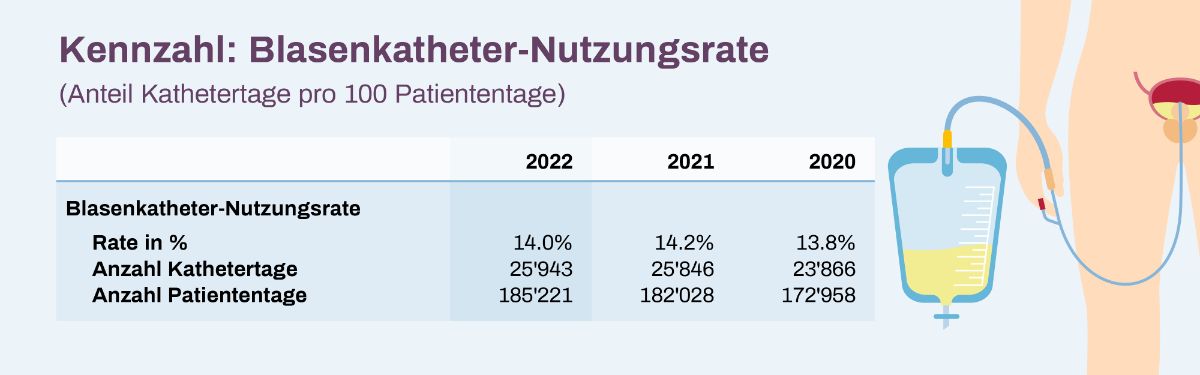
Source: USB, internal evaluations of all wards excluding: day clinics, emergency center, intensive care unit, IMC, neurosurgical monitoring unit
Treatment outcome from the patient's perspective (PROMs)
As part of our quality measurements, we place a special focus on the treatment outcome from the patient's perspective. You can find out more about the so-called PROMs - Patient Reported Outcome Measures - here.
Patient opinion
Data on how patients rate the USB can be found here.
